Anatomy of the anterior chest wall. “Topographic anatomy and operative surgery of the chest walls, breast
1. Upper - along the jugular notch, along the upper edge of the clavicles, clavicular-acromial joints and along conditional lines drawn from this joint to the spinous process of the VII cervical vertebra.
2. Lower - from the base of the xiphoid process, along the edges of the costal arches to the X ribs, from where along conventional lines through the free ends of the XI and XII ribs to the spinous process of the XII thoracic vertebra. The chest area is separated from the upper limbs on the left and right by a line running anteriorly along the deltoid-pectoral groove, and posteriorly along the medial edge of the deltoid muscle.
Layer-by-layer topography of the chest wall along the midclavicular line
1. The skin on the anterior surface is thinner than in the back area, contains sebaceous and sweat glands, and is easily mobile with the exception of the sternum and posterior median area.
2. Subcutaneous fatty tissue is more developed in women, contains a dense venous network, numerous arteries, which are branches of the internal thoracic, lateral thoracic and posterior intercostal arteries, superficial nerves originating from the intercostal and supraclavicular nerves of the cervical plexus.
3. The superficial fascia in women forms the capsule of the mammary gland.
4. Mammary gland
5. The proper fascia (pectoral fascia) consists of two layers - superficial and deep (cleidopectoral fascia), forming fascial sheaths for the pectoralis major and minor muscles, and on the posterior wall for the lower part of the trapezius muscle and the latissimus dorsi muscle. In the area of the sternum, the fascia passes into the anterior aponeurotic plate, which is fused with the periosteum (there is no muscle layer in this area).
6. Pectoralis major muscle.
7. Superficial subpectoral cellular space.
8. Pectoralis minor muscle.
9. Deep subpectoral cellular space – subpectoral phlegmons can develop in these spaces.
10. Intercostal space is a complex of formations (muscles, vessels, nerves) located between two adjacent ribs.
The most superficially located external intercostal muscles, which fill the intercostal space from the tubercles of the ribs to the outer ends of the costal cartilages. In the area of the costal cartilages, the muscles are replaced by fibrous fibers of the external intercostal membrane. The fibers of the external intercostal muscles run in the direction from top to bottom and from back to front.
Deeper than the external ones are the internal intercostal muscles, the direction of the fibers of which is opposite to the movement of the external intercostal muscles, i.e. from bottom to top and back to front. The internal intercostal muscles occupy the intercostal spaces from the corners of the ribs to the sternum. From the corners of the ribs to the spinal column they are replaced by a thin internal intercostal membrane. The space between the external and internal intercostal muscles is made of a thin layer of loose fiber, in which intercostal vessels and nerves pass.
Intercostal arteries can be divided into anterior and posterior. The anterior arteries are branches of the internal mammary artery. The posterior intercostal arteries, except for the two upper ones, which arise from the costocervical trunk of the subclavian artery, begin from the thoracic aorta.
The intercostal vein is located above, and the intercostal nerve is located below the artery. From the corners of the ribs to the mid-axillary line, the intercostal vessels are hidden behind the lower edge of the rib, the nerve passes along this edge. Anterior to the midaxillary line, the intercostal neurovascular bundle emerges from under the lower edge of the rib. Guided by the structure of the intercostal space, it is advisable to carry out punctures of the chest in the VII-VIII intercostal space between the scapular and middle axillary lines along the upper edge of the underlying rib.
11. The intrathoracic fascia is more pronounced in the anterior and lateral areas of the chest wall, less so near the spinal column.
12. Prepleural tissue.
13. Pleura.
Breast
Skeletotopy: between the III and VI ribs above and below and between the parasternal and anterior axillary lines on the sides.
Structure. Consists of 15–20 lobules surrounded and separated by processes of the superficial fascia. The lobules of the gland are located radially around the nipple. Each lobule has its own excretory, or lacteal, duct with a diameter of 2–3 mm. The milk ducts converge radially towards the nipple and at its base expand in an ampulla-like manner, forming milk sinuses, which narrow outwards again and open at the top of the nipple with pinholes. The number of holes on the nipple is usually less than the number of milk ducts, since some of them are connected to each other at the base of the nipple.
Blood supply: branches of the internal thoracic, lateral thoracic, intercostal arteries. The deep veins accompany the arteries of the same name, the superficial ones form a subcutaneous network, individual branches of which flow into the axillary vein.
Innervation: lateral branches of the intercostal nerves, branches of the cervical and brachial plexuses.
Lymphatic drainage. The lymphatic system of the female mammary gland and the location of regional lymph nodes are of great practical interest due to the frequent damage to the organ by a malignant process.
The main route of lymph outflow is to the axillary lymph nodes in three directions:
1. through the anterior thoracic lymph nodes (Zorgius and Bartels) along the outer edge of the pectoralis major muscle at the level of the second or third rib;
2. intrapectorally – through Rotter’s nodes between the pectoralis major and minor muscles;
3. transpectorally - along the lymphatic vessels piercing the thickness of the pectoralis major and minor muscles; nodes are located between their fibers.
Additional pathways for lymph outflow:
1. from the medial section - to the lymph nodes along the internal mammary artery and anterior mediastinum;
2. from the upper section - to the subclavian and supraclavicular nodes;
3. from the lower section - to the nodes of the abdominal cavity.
Diaphragm
The diaphragm is a muscular-fascial formation, the basis of which is a wide, relatively thin muscle, shaped like a dome, the convexity of which faces upward towards the chest cavity. The diaphragm is represented by two sections: tendon and muscle.
The tendon part forms the right and left domes, as well as an indentation from the heart. It distinguishes between the right and left lateral, as well as the anterior sections. In the anterior section there is an opening for the inferior vena cava.
The muscular section of the diaphragm, according to the points of its fixation around the circumference of the lower aperture of the chest, is divided into three parts: lumbar, sternal and costal.
1. The lumbar part begins from the four upper lumbar vertebrae with two legs - right and left, which, forming a cross in the form of the number 8, form two openings: the aortic, through which the descending part of the aorta and the thoracic lymphatic duct pass, and the esophageal - the esophagus and vagus trunks . Between the muscle bundles on the sides of the legs of the diaphragm pass the azygos, semi-gypsy veins and splanchnic nerves, as well as the sympathetic trunk.
2. The sternal part begins from the inner surface of the xiphoid process of the sternum.
3. The costal part starts from the VII-XII ribs.
Weak spots:
1. lumbar-costal triangles (Bochdalek) – waiting for the lumbar and costal parts of the diaphragm;
2. sternocostal triangles (right – Morgarya’s fissure, left – Larrey’s fissure) – between the sternum and costal parts of the diaphragm.
In these muscle gaps the layers of the intrathoracic and intra-abdominal fascia come into contact. These areas of the diaphragm can be the site of formation of diaphragmatic hernias, and when the fascia is destroyed by the suppurative process, it becomes possible for it to pass from the subpleural tissue to the subperitoneal tissue and back. The esophageal opening is also a weak point of the diaphragm.
Blood supply: internal thoracic, superior and inferior phrenic, intercostal arteries.
Innervation: phrenic, intercostal, vagus and sympathetic nerves.
Mediastinum
The mediastinum is a space made up of a complex of organs and neurovascular formations, limited on the sides by the mediastinal pleura, in front, behind and below by the intrathoracic fascia, behind which the sternum is located in front, behind - the spinal column, below - the diaphragm.
Classification:
1. The superior mediastinum includes all anatomical formations lying above the conventional horizontal plane drawn at the level of the upper edge of the roots of the lungs.
Contents: aortic arch; brachiocephalic trunk; left common carotid artery; left subclavian artery; thymus; brachiocephalic veins; superior vena cava; phrenic nerves; vagus nerves; recurrent laryngeal nerves; trachea; esophagus; thoracic lymphatic duct; paratracheal, upper and lower tracheobronchial lymph nodes.
2. The anterior mediastinum is located below the indicated plane, between the sternum and the pericardium.
Contents: loose fiber; parasternal and superior diaphragmatic lymph nodes; thymus gland and intrathoracic arteries.
3. Middle mediastinum
Contents: pericardium; heart; ascending aorta; pulmonary trunk; pulmonary arteries and pulmonary veins; right and left main bronchi; upper segment of the superior vena cava; right and left phrenic nerves; pericardial phrenic arteries and veins; lymph nodes and tissue.
4. The posterior mediastinum is located between the pericardium and the vertebral column.
Contents: descending aorta; esophagus; vagus nerves; borderline sympathetic trunk and greater and lesser splanchnic nerves; azygos vein; hemizygos vein; accessory hemizygos vein; thoracic lymphatic duct; lymph nodes and tissue.
The pleura forms two serous sacs. Between the two layers of the pleura - visceral and parietal - there is a slit-like space called the pleural cavity. Depending on the area that the parietal pleura lines, it is divided into:
1. costal,
2. diaphragmatic,
3. mediastinal pleura.
The parts of the pleural cavity that are located at the junction of one section of the parietal pleura to another are called pleural sinuses:
1. costophrenic sinus;
2. costomediastinal sinus;
3. phrenic-mediastinal sinus.
In each lung there are three surfaces: the outer, or costal, diaphragmatic and medial.
Each lung is divided into lobes. The right lung has three lobes - upper, middle and lower, and the left lung has two lobes - upper and lower. The lungs are also divided into segments. A segment is a section of the lung ventilated by a third-order bronchus. Each lung has 10 segments.
The hilum is located on the medial surface of each lung. Here are the anatomical formations that make up the root of the lung: the bronchus, pulmonary arteries and veins, bronchial vessels and nerves, lymph nodes. Skeletotopically, the root of the lung is located at the level of the V-VII thoracic vertebrae.
Syntopy of the lung root components
1. From top to bottom: in the right lung - main bronchus, pulmonary artery, pulmonary veins; in the left - the pulmonary artery, main bronchus, pulmonary veins. (BAV, ABC)
2. From front to back - veins are located in both lungs, then the artery and the bronchus occupy the posterior position. (VAB) Pericardium
The pericardium is a closed serous sac that surrounds the heart, the ascending part of the aorta before it passes into the arch, the pulmonary trunk to the place of its division, and the openings of the vena cava and pulmonary veins.
The pericardium has layers:
1. external (fibrous);
2. internal (serous):
Parietal plate;
Visceral plate (epicardium) - covers the surface of the heart.
In those places where the epicardium passes into the parietal plate of the serous pericardium, sinuses are formed:
1. transverse, located in the area of the ascending aorta and pulmonary trunk;
2. oblique – located in the lower part of the posterior pericardium;
3. anterior-inferior, located in the place where the pericardium enters the angle between the diaphragm and the anterior chest wall.
Topographic anatomy and operative surgery of the chest wall and organs of the thoracic cavity Lecturer - Art. teacher S. I. Veretennikov
 Boundaries of the chest wall At the top - the jugular notch of the sternum, the clavicle and the line from its acromial end to the spinous process of the VII cervical vertebra; Below - a line from the xiphoid process along the edge of the costal arch and along the XII rib to the XII thoracic vertebra; On the sides: in front along the line of sulcus deltoideopectoralis, in back - along the medial edge of m. deltoideus
Boundaries of the chest wall At the top - the jugular notch of the sternum, the clavicle and the line from its acromial end to the spinous process of the VII cervical vertebra; Below - a line from the xiphoid process along the edge of the costal arch and along the XII rib to the XII thoracic vertebra; On the sides: in front along the line of sulcus deltoideopectoralis, in back - along the medial edge of m. deltoideus
 Lines of the chest wall 1 linea axillaris posterior; 2 linea axillaris media; 3 linea axillaris anterior; 4 linea medioclavicularis; 5 linea parasternalis; 6 linea sternalis; 7 linea mediana anterior; 8 linea mediana posterior; 9 linea vertebralis; 10 linea paravertebralis; 11 linea scapularis.
Lines of the chest wall 1 linea axillaris posterior; 2 linea axillaris media; 3 linea axillaris anterior; 4 linea medioclavicularis; 5 linea parasternalis; 6 linea sternalis; 7 linea mediana anterior; 8 linea mediana posterior; 9 linea vertebralis; 10 linea paravertebralis; 11 linea scapularis.
 Breast shapes Wide and short chest Narrow and long chest epigastric angle more than 100 degrees wide intercostal spaces and sternum epigastric angle less than 100 degrees, narrow intercostal spaces and sternum
Breast shapes Wide and short chest Narrow and long chest epigastric angle more than 100 degrees wide intercostal spaces and sternum epigastric angle less than 100 degrees, narrow intercostal spaces and sternum
 The shape of the chest in children under 3 years of age - cone with the base down by 5 years - cylindrical by 7 years - cone with the base up by 12-13 years - the formation of the chest ends
The shape of the chest in children under 3 years of age - cone with the base down by 5 years - cylindrical by 7 years - cone with the base up by 12-13 years - the formation of the chest ends
 Age-related features of the chest: ribs are located horizontally up to 3 years of age 3 free ribs By 5-6 years of age, a rib groove begins to form By 12 years of age, the intercostal neurovascular bundle is hidden in the groove The jugular notch of the sternum is projected at the level of the upper edge of Th I, by 7 years of age - Th II
Age-related features of the chest: ribs are located horizontally up to 3 years of age 3 free ribs By 5-6 years of age, a rib groove begins to form By 12 years of age, the intercostal neurovascular bundle is hidden in the groove The jugular notch of the sternum is projected at the level of the upper edge of Th I, by 7 years of age - Th II
 Funnel chest deformity Shoemaker's chest (pectus excavatum) curvature of the sternum and anterior ribs, leading to a decrease in the sternum-vertebral distance, chest volume, compression and displacement of the mediastinal organs, causing functional disorders of the cardiovascular and respiratory systems.
Funnel chest deformity Shoemaker's chest (pectus excavatum) curvature of the sternum and anterior ribs, leading to a decrease in the sternum-vertebral distance, chest volume, compression and displacement of the mediastinal organs, causing functional disorders of the cardiovascular and respiratory systems.
 Gizycka index for determining the degree of chest deformation I degree more than 0.7 II degree from 0.7 to 0.5 III degree less than 0.5
Gizycka index for determining the degree of chest deformation I degree more than 0.7 II degree from 0.7 to 0.5 III degree less than 0.5
 Methods of surgical treatment of VDHA Without fixators of the sternocostal complex With the use of external fixators With the use of internal fixators Operations to invert the sternum by 180°
Methods of surgical treatment of VDHA Without fixators of the sternocostal complex With the use of external fixators With the use of internal fixators Operations to invert the sternum by 180°
 Operations without fixators of the sternocostal complex (Thoracoplasty according to Ravitch M.) a) removal of costal cartilages, cutting off b) sternotomy and installation of a cartilaginous spacer in the area of sternotomy. xiphoid process; fixation of the second costal cartilage in the form of a “tile”
Operations without fixators of the sternocostal complex (Thoracoplasty according to Ravitch M.) a) removal of costal cartilages, cutting off b) sternotomy and installation of a cartilaginous spacer in the area of sternotomy. xiphoid process; fixation of the second costal cartilage in the form of a “tile”
 Operations without fixators of the sternocostal complex (Thoracoplasty according to N. I. Kondrashin) a) skin incision line; b) excision of cartilage and wedge-shaped chondrotomy; wedge and transverse sternotomy
Operations without fixators of the sternocostal complex (Thoracoplasty according to N. I. Kondrashin) a) skin incision line; b) excision of cartilage and wedge-shaped chondrotomy; wedge and transverse sternotomy

 Operations for inverting the sternum by 180 degrees Operation according to Wada (free inversion of the sternum) Operation according to Jung A (inversion of the sternum on a muscular pedicle) Operation according to Taguchi K. (inversion of the sternum with preservation of the vascular bundle)
Operations for inverting the sternum by 180 degrees Operation according to Wada (free inversion of the sternum) Operation according to Jung A (inversion of the sternum on a muscular pedicle) Operation according to Taguchi K. (inversion of the sternum with preservation of the vascular bundle)
 Operations using internal fixators Thoracoplasty according to Rehbein F. Thoracoplasty according to Paltia V. and Sulamaa M.
Operations using internal fixators Thoracoplasty according to Rehbein F. Thoracoplasty according to Paltia V. and Sulamaa M.
 The most optimal methods are operations using internal fixation devices: less traumatic, easier to tolerate by patients, does not interfere with leading an active lifestyle, the rehabilitation period is shorter
The most optimal methods are operations using internal fixation devices: less traumatic, easier to tolerate by patients, does not interfere with leading an active lifestyle, the rehabilitation period is shorter
 Results of treatment of stage III pectus excavatum deformity a) before surgery b) 6 months after surgery
Results of treatment of stage III pectus excavatum deformity a) before surgery b) 6 months after surgery


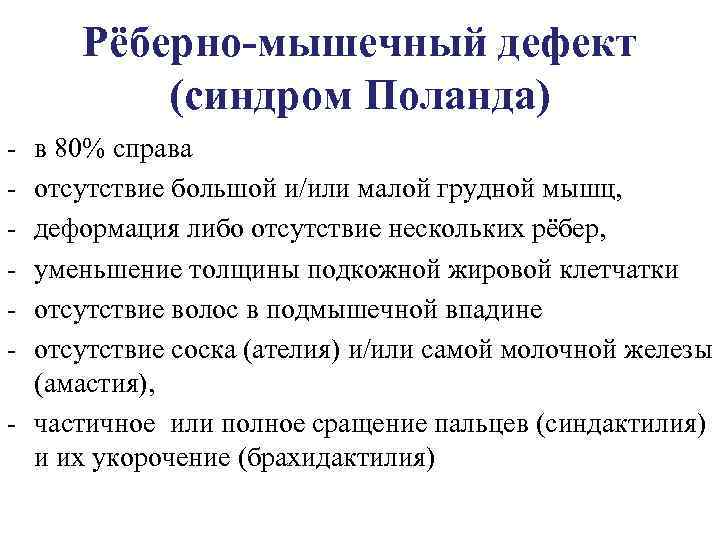 Costomuscular defect (Poland syndrome) in 80% on the right, absence of the pectoralis major and/or minor muscles, deformation or absence of several ribs, decreased thickness of the subcutaneous fatty tissue, absence of hair in the armpit, absence of the nipple (atelia) and/or the mammary gland itself (amastia ), partial or complete fusion of the fingers (syndactyly) and their shortening (brachydactyly)
Costomuscular defect (Poland syndrome) in 80% on the right, absence of the pectoralis major and/or minor muscles, deformation or absence of several ribs, decreased thickness of the subcutaneous fatty tissue, absence of hair in the armpit, absence of the nipple (atelia) and/or the mammary gland itself (amastia ), partial or complete fusion of the fingers (syndactyly) and their shortening (brachydactyly)


 Development of the diaphragm Primary diaphragm - formed at 4-6 weeks in the form of a connective tissue septum from the mesoderm Secondary diaphragm - formed by the 3rd month due to the ingrowth of myomeres (muscle tissue) into the connective tissue plate
Development of the diaphragm Primary diaphragm - formed at 4-6 weeks in the form of a connective tissue septum from the mesoderm Secondary diaphragm - formed by the 3rd month due to the ingrowth of myomeres (muscle tissue) into the connective tissue plate
 Diaphragmatic hernia If development is disrupted at the stage of the primary diaphragm, a defect remains in the diaphragm and a false diaphragmatic hernia is formed (usually in the costovertebral region, Bogdalek’s hernia). If development is disrupted at the stage of the secondary diaphragm, myomeres do not germinate, connective tissue weak points are preserved, and a true diaphragmatic hernia is formed.
Diaphragmatic hernia If development is disrupted at the stage of the primary diaphragm, a defect remains in the diaphragm and a false diaphragmatic hernia is formed (usually in the costovertebral region, Bogdalek’s hernia). If development is disrupted at the stage of the secondary diaphragm, myomeres do not germinate, connective tissue weak points are preserved, and a true diaphragmatic hernia is formed.
 Classification of diaphragmatic hernias 1. Congenital diaphragmatic hernias: diaphragmatic pleural hiatal hernias parasternal phrenopericardial 2. Acquired diaphragmatic hernias: traumatic
Classification of diaphragmatic hernias 1. Congenital diaphragmatic hernias: diaphragmatic pleural hiatal hernias parasternal phrenopericardial 2. Acquired diaphragmatic hernias: traumatic

 Methods of surgical treatment of diaphragmatic hernias 1. Hiatoplasty - suturing the hernial orifice with U-shaped sutures to the left and right of the esophagus 2. Diaphragmcrurorrhaphy - suturing the legs of the diaphragm behind the esophagus 3. Gastropexy - after moving the stomach into the abdominal cavity, its fixation to the anterior abdominal wall in combination with narrowing esophageal opening With the radical method, the following is carried out: reduction and fixation of the stomach in the abdominal cavity, creation of an acute angle of His, narrowing of the dilated esophageal opening of the diaphragm. These methods include: 1. Esophagofundopexy - the fundus of the stomach is sutured to the wall of the esophagus. The second row is to the anterior surface of the esophagus, as a result of which the fundus of the stomach covers the abdominal section of the esophagus by 23, forming an acute angle between them. The fundus of the stomach is then sutured to the lower surface of the diaphragm. 2. Nissen fundoplication – a sleeve is formed around the esophagus with the bottom of the stomach.
Methods of surgical treatment of diaphragmatic hernias 1. Hiatoplasty - suturing the hernial orifice with U-shaped sutures to the left and right of the esophagus 2. Diaphragmcrurorrhaphy - suturing the legs of the diaphragm behind the esophagus 3. Gastropexy - after moving the stomach into the abdominal cavity, its fixation to the anterior abdominal wall in combination with narrowing esophageal opening With the radical method, the following is carried out: reduction and fixation of the stomach in the abdominal cavity, creation of an acute angle of His, narrowing of the dilated esophageal opening of the diaphragm. These methods include: 1. Esophagofundopexy - the fundus of the stomach is sutured to the wall of the esophagus. The second row is to the anterior surface of the esophagus, as a result of which the fundus of the stomach covers the abdominal section of the esophagus by 23, forming an acute angle between them. The fundus of the stomach is then sutured to the lower surface of the diaphragm. 2. Nissen fundoplication – a sleeve is formed around the esophagus with the bottom of the stomach.
 Fundoplication according to Nissen a) creation of an artificial ligamentous apparatus with the formation of an acute angle of His b) final appearance of the formed cuff around the esophagus
Fundoplication according to Nissen a) creation of an artificial ligamentous apparatus with the formation of an acute angle of His b) final appearance of the formed cuff around the esophagus
 Topographic anatomy of the pleura Layers of the pleura: parietal layer, visceral layer. Sections of the pleura: costal pleura, diaphragmatic pleura, mediastinal pleura. Sinuses of the pleura: costal diaphragmatic (lower section of the pleural cavity - the place of fluid accumulation); costal mediastinal: left anterior is usually projected near the left edge of the sternum; the front right is located near the midline on the left; diaphragmatic mediastinal – performed entirely by the lungs during inhalation
Topographic anatomy of the pleura Layers of the pleura: parietal layer, visceral layer. Sections of the pleura: costal pleura, diaphragmatic pleura, mediastinal pleura. Sinuses of the pleura: costal diaphragmatic (lower section of the pleural cavity - the place of fluid accumulation); costal mediastinal: left anterior is usually projected near the left edge of the sternum; the front right is located near the midline on the left; diaphragmatic mediastinal – performed entirely by the lungs during inhalation
 Projection of the borders of the lungs, their lobes and the parietal pleura onto the chest (front view) 1 lower lobes of the right and left lungs; 2 middle lobe of the right lung; 3 upper lobes of the right and left lung
Projection of the borders of the lungs, their lobes and the parietal pleura onto the chest (front view) 1 lower lobes of the right and left lungs; 2 middle lobe of the right lung; 3 upper lobes of the right and left lung
 The dome of the pleura is a section of the parietal pleura protruding above the upper aperture of the chest and fixed by the costal pleural and vertebral pleural ligaments. Laterally and superiorly - adjacent to the scalene muscles Medially and posteriorly - to the trachea and esophagus Anteriorly to the subclavian artery and vein Superiorly - to the brachial plexus
The dome of the pleura is a section of the parietal pleura protruding above the upper aperture of the chest and fixed by the costal pleural and vertebral pleural ligaments. Laterally and superiorly - adjacent to the scalene muscles Medially and posteriorly - to the trachea and esophagus Anteriorly to the subclavian artery and vein Superiorly - to the brachial plexus
 Types of pneumothorax By origin: traumatic spontaneous artificial By air volume: limited full By communication with the external environment open closed valve
Types of pneumothorax By origin: traumatic spontaneous artificial By air volume: limited full By communication with the external environment open closed valve

 Emergency care for open pneumothorax First aid is the application of an aseptic occlusive dressing to the wound, vagosympathetic blockade. Surgical treatment: primary surgical treatment of the wound and sealing of the pleural cavity: wound suturing method: application of pleuromuscular sutures, application of intercostal sutures (polysal suture), subperiosteal resection of the rib. the use of plastic methods: plastic surgery with a muscle flap on a leg, a diaphragm, the edge of the lung, a patch made of synthetic material.
Emergency care for open pneumothorax First aid is the application of an aseptic occlusive dressing to the wound, vagosympathetic blockade. Surgical treatment: primary surgical treatment of the wound and sealing of the pleural cavity: wound suturing method: application of pleuromuscular sutures, application of intercostal sutures (polysal suture), subperiosteal resection of the rib. the use of plastic methods: plastic surgery with a muscle flap on a leg, a diaphragm, the edge of the lung, a patch made of synthetic material.
 Wound treatment for open pneumothorax Resection of rib ends Closure of a wound defect of the chest wall using a pedicle muscle flap
Wound treatment for open pneumothorax Resection of rib ends Closure of a wound defect of the chest wall using a pedicle muscle flap


 Hemothorax (accumulation of blood in the pleural cavity) Classification according to P. A. Kupriyanov: Small hemothorax - within the costophrenic sinus Medium hemothorax - up to the level of the angle of the scapula Large hemothorax - above the angle of the scapula
Hemothorax (accumulation of blood in the pleural cavity) Classification according to P. A. Kupriyanov: Small hemothorax - within the costophrenic sinus Medium hemothorax - up to the level of the angle of the scapula Large hemothorax - above the angle of the scapula
 Puncture of the pleural cavity for hydrothorax A) position of the patient during puncture B) puncture along the upper edge of the underlying rib so as not to damage the intercostal neurovascular bundle
Puncture of the pleural cavity for hydrothorax A) position of the patient during puncture B) puncture along the upper edge of the underlying rib so as not to damage the intercostal neurovascular bundle
 Puncture of the pleural cavity for hydrothorax Puncture with a Dufault needle in the 7-8 intercostal space between the scapular and posterior axillary lines with a rubber valve (drainage according to N. N. Petrov), subsequently with active aspiration.
Puncture of the pleural cavity for hydrothorax Puncture with a Dufault needle in the 7-8 intercostal space between the scapular and posterior axillary lines with a rubber valve (drainage according to N. N. Petrov), subsequently with active aspiration.
 Complications during pleural puncture 1 needle is inserted into the lung tissue; 2 the needle is inserted into the pleural cavity above the fluid level; 3 the needle is inserted into the fusion between the layers of the pleura of the costal phrenic sinus; 4, the needle is inserted through the costal phrenic sinus and the diaphragm into the abdominal cavity.
Complications during pleural puncture 1 needle is inserted into the lung tissue; 2 the needle is inserted into the pleural cavity above the fluid level; 3 the needle is inserted into the fusion between the layers of the pleura of the costal phrenic sinus; 4, the needle is inserted through the costal phrenic sinus and the diaphragm into the abdominal cavity.
 Resection of the rib Separation of the periosteum from the upper and lower edges of the rib Separation of the periosteum from the inner surface of the rib and intersection of the rib
Resection of the rib Separation of the periosteum from the upper and lower edges of the rib Separation of the periosteum from the inner surface of the rib and intersection of the rib
 Drainage of the pleural cavity Indications: hemothorax, pyothorax, chylothorax. Surgical procedure: a skin incision (1 cm) in the 7 m intercostal space along the posterior axillary line, a trocar is inserted, the stylet is removed, drainage is performed (latex or silicone tube) and a system for active aspiration is connected.
Drainage of the pleural cavity Indications: hemothorax, pyothorax, chylothorax. Surgical procedure: a skin incision (1 cm) in the 7 m intercostal space along the posterior axillary line, a trocar is inserted, the stylet is removed, drainage is performed (latex or silicone tube) and a system for active aspiration is connected.
 Anterolateral thoracotomy access through the 4th (5–6) intercostal space, incision along the upper edge of the underlying rib, 2 cm does not reach the sternum
Anterolateral thoracotomy access through the 4th (5–6) intercostal space, incision along the upper edge of the underlying rib, 2 cm does not reach the sternum

 Posterolateral thoracotomy Position: prone or semilateral. Incision: at the level of 3 4 thoracic vertebrae along the paravertebral line to the angle of the scapula, then bending around the scapula to the anterior axillary line
Posterolateral thoracotomy Position: prone or semilateral. Incision: at the level of 3 4 thoracic vertebrae along the paravertebral line to the angle of the scapula, then bending around the scapula to the anterior axillary line
 Longitudinal median sternotomy The midline incision begins 2 cm above the manubrium of the sternum and continues 3 cm below the xiphoid process
Longitudinal median sternotomy The midline incision begins 2 cm above the manubrium of the sternum and continues 3 cm below the xiphoid process

 Transverse combined transbipleural approach Bilateral thoracotomy along the 6th intercostal space on the right, with transverse intersection of the sternum at the level of the intercostal space and continuation of thoracotomy along the 6th intercostal space on the left
Transverse combined transbipleural approach Bilateral thoracotomy along the 6th intercostal space on the right, with transverse intersection of the sternum at the level of the intercostal space and continuation of thoracotomy along the 6th intercostal space on the left

 Topography of the esophagus The cervical vertebra, pars cervicalis, is located from the level of the VI cervical vertebra to the I–II thoracic vertebra. Its length ranges from 5 to 8 cm. The thoracic part, pars thoracica, has the greatest length - 15-18 cm and ends at the level of the IX-X thoracic vertebrae at the point where the esophagus enters the esophageal opening of the diaphragm. The abdominal part, pars abdominalis - from the esophageal opening of the diaphragm to the cardial opening of the stomach, the shortest (1-3 cm). 4 bends: two in the sagittal plane and two in the frontal plane.
Topography of the esophagus The cervical vertebra, pars cervicalis, is located from the level of the VI cervical vertebra to the I–II thoracic vertebra. Its length ranges from 5 to 8 cm. The thoracic part, pars thoracica, has the greatest length - 15-18 cm and ends at the level of the IX-X thoracic vertebrae at the point where the esophagus enters the esophageal opening of the diaphragm. The abdominal part, pars abdominalis - from the esophageal opening of the diaphragm to the cardial opening of the stomach, the shortest (1-3 cm). 4 bends: two in the sagittal plane and two in the frontal plane.
 Constrictions of the esophagus 3 narrowings: a – at the place where the pharynx enters the esophagus, (15 cm from the edge of the teeth) b – at the place where the esophagus is adjacent to the aortic arch, (25 cm from the edge of the teeth) c – at the place where the diaphragm passes through the esophageal opening – physiological cardiac sphincter (38 cm from the edge of the teeth)
Constrictions of the esophagus 3 narrowings: a – at the place where the pharynx enters the esophagus, (15 cm from the edge of the teeth) b – at the place where the esophagus is adjacent to the aortic arch, (25 cm from the edge of the teeth) c – at the place where the diaphragm passes through the esophageal opening – physiological cardiac sphincter (38 cm from the edge of the teeth)
 Thoracic part of the esophagus Syntopy: - the upper third (level TIII) is closed in front by the trachea, connecting to it by connective tissue bridges - the middle third (TIV VI) in front is the aortic arch, tracheal bifurcation and left ch. bronchus - lower third (TVII TX) parallel to the aorta, at the diaphragm the esophagus bends to the left
Thoracic part of the esophagus Syntopy: - the upper third (level TIII) is closed in front by the trachea, connecting to it by connective tissue bridges - the middle third (TIV VI) in front is the aortic arch, tracheal bifurcation and left ch. bronchus - lower third (TVII TX) parallel to the aorta, at the diaphragm the esophagus bends to the left
 Innervation: plexus esophageus (n. vagus and truncus sympathicus) Blood supply: cervical part - rr. esophageales from a. thyreoidea inferior; chest part – rr. esophageales or aorta thoracica, abdominal part – rr. esophageales from a. gastrica sinistra and a. phrenica inferior sinistra. Venous outflow: from the cervical part to v. thyreoidea inferior, and then in v. brachiocephalica; from the thoracic part - in v. azygos and v. hemiazygos; from the abdominal part - in v. gastrica sinistra, and then in v. portae. Lymphatic drainage: from the cervical part to the nodi lymphatici tracheobronchiales superiores et inferiores, paratracheales and paraverlebrales; from the thoracic part - in the nodi lymphatici tracheobronchiales inferiores and mediastinals posteriores: from the abdominal part - in the anulus lymphatici cardii.
Innervation: plexus esophageus (n. vagus and truncus sympathicus) Blood supply: cervical part - rr. esophageales from a. thyreoidea inferior; chest part – rr. esophageales or aorta thoracica, abdominal part – rr. esophageales from a. gastrica sinistra and a. phrenica inferior sinistra. Venous outflow: from the cervical part to v. thyreoidea inferior, and then in v. brachiocephalica; from the thoracic part - in v. azygos and v. hemiazygos; from the abdominal part - in v. gastrica sinistra, and then in v. portae. Lymphatic drainage: from the cervical part to the nodi lymphatici tracheobronchiales superiores et inferiores, paratracheales and paraverlebrales; from the thoracic part - in the nodi lymphatici tracheobronchiales inferiores and mediastinals posteriores: from the abdominal part - in the anulus lymphatici cardii.
 Malformations of the esophagus: esophageal atresia (treatment method depends on the distance between the blind ends of the esophagus) esophageal tracheal fistulas (usually in the middle or lower third, treatment method depends on the diameter of the fistula) cardiostenosis diverticula
Malformations of the esophagus: esophageal atresia (treatment method depends on the distance between the blind ends of the esophagus) esophageal tracheal fistulas (usually in the middle or lower third, treatment method depends on the diameter of the fistula) cardiostenosis diverticula
 Cardiostenosis, achalasia of the cardia According to B.V. Petrovsky (1957), he distinguishes four stages of the disease: I functional spasm without dilatation of the esophagus; II persistent spasm with moderate dilatation of the esophagus; III cicatricial changes in the muscle layers with pronounced expansion of the esophagus; IV cardiostenosis with a large expansion of the esophagus and its S-shaped curvature.
Cardiostenosis, achalasia of the cardia According to B.V. Petrovsky (1957), he distinguishes four stages of the disease: I functional spasm without dilatation of the esophagus; II persistent spasm with moderate dilatation of the esophagus; III cicatricial changes in the muscle layers with pronounced expansion of the esophagus; IV cardiostenosis with a large expansion of the esophagus and its S-shaped curvature.
 Treatment of cardiac stenosis Conservative Instrumental (cardiodilation) causes stretching and partial damage to the circular muscles and myoneural connections. hydraulic cardiodilators pneumatic cardiodilators mechanical cardiodilators (Stark) Surgical
Treatment of cardiac stenosis Conservative Instrumental (cardiodilation) causes stretching and partial damage to the circular muscles and myoneural connections. hydraulic cardiodilators pneumatic cardiodilators mechanical cardiodilators (Stark) Surgical
 Surgical treatment of cardiac stenosis is extramucosal esophagocardiomyotomy, which consists of dissecting only the muscular layer of the esophagus to the mucous membrane (Gottstein 1901, Heller 1913). myotomy according to Geller, myotomy with plastic surgery of the formed defect with a diaphragm flap (B.V. Petrovsky 1949), omentum (I.M. Chuikov 1932), stomach (T.A. Suvorova 1960, A.A. Shalimov 1976). extramucosal esophagocardiomyotomy with plasty of the esophagus using the anterior wall of the stomach (Gottstein Geller Suvorova operation) from thoracotomy access. resection of the thoracic esophagus and cardia of the stomach with simultaneous gastric plasty for achalasia cardia stages III and IV (B. I. Miroshnikov et al., 2001). Satisfactory results of surgical treatment of cardiac stenosis were obtained in 80–87% of patients. The mortality rate is about 1%.
Surgical treatment of cardiac stenosis is extramucosal esophagocardiomyotomy, which consists of dissecting only the muscular layer of the esophagus to the mucous membrane (Gottstein 1901, Heller 1913). myotomy according to Geller, myotomy with plastic surgery of the formed defect with a diaphragm flap (B.V. Petrovsky 1949), omentum (I.M. Chuikov 1932), stomach (T.A. Suvorova 1960, A.A. Shalimov 1976). extramucosal esophagocardiomyotomy with plasty of the esophagus using the anterior wall of the stomach (Gottstein Geller Suvorova operation) from thoracotomy access. resection of the thoracic esophagus and cardia of the stomach with simultaneous gastric plasty for achalasia cardia stages III and IV (B. I. Miroshnikov et al., 2001). Satisfactory results of surgical treatment of cardiac stenosis were obtained in 80–87% of patients. The mortality rate is about 1%.
 Esophageal diverticula 1. Pharyngeal esophageal diverticula (63%) simultaneous diverticulectomy from an incision along the inner edge of the sternocleidomastoid muscle on the left.) 2. Epiphrenal (20%) diverticulectomy, most often from the right thoracotomy approach. 3. Bifurcation (17%) simultaneous diverticulectomy or invagination of the diverticulum from the right transpleural approach
Esophageal diverticula 1. Pharyngeal esophageal diverticula (63%) simultaneous diverticulectomy from an incision along the inner edge of the sternocleidomastoid muscle on the left.) 2. Epiphrenal (20%) diverticulectomy, most often from the right thoracotomy approach. 3. Bifurcation (17%) simultaneous diverticulectomy or invagination of the diverticulum from the right transpleural approach
 Operations on the esophagus Esophagotomy – dissection of the esophagus. To remove foreign bodies and eliminate congenital strictures. Dobromyslov-Torek operation. When the tumor is located in the middle third. Access – right-sided, transpleural. Resection of the esophagus, immersion of the lower stump into the stomach, and the proximal stump into the neck. Creation of a gastric stoma. Resection of the lower third of the esophagus with anastomosis or its replacement with the gastric wall along the greater curvature (Gavrilov operation). Anastomosis with the small intestine. Esophagoplasty – replacement of the esophagus with the small or large intestine (antethoracic plastic surgery according to Ru Herzen Yudin).
Operations on the esophagus Esophagotomy – dissection of the esophagus. To remove foreign bodies and eliminate congenital strictures. Dobromyslov-Torek operation. When the tumor is located in the middle third. Access – right-sided, transpleural. Resection of the esophagus, immersion of the lower stump into the stomach, and the proximal stump into the neck. Creation of a gastric stoma. Resection of the lower third of the esophagus with anastomosis or its replacement with the gastric wall along the greater curvature (Gavrilov operation). Anastomosis with the small intestine. Esophagoplasty – replacement of the esophagus with the small or large intestine (antethoracic plastic surgery according to Ru Herzen Yudin).

 Resection of the esophagus Isolation of the esophagus with surrounding tissue and lymph nodes from the posterior mediastinum Separation of the anterior wall of the esophagus from the pericardium.
Resection of the esophagus Isolation of the esophagus with surrounding tissue and lymph nodes from the posterior mediastinum Separation of the anterior wall of the esophagus from the pericardium.
 Resection of the esophagus Separation of the posterior wall of the esophagus from the aorta Crossing and ligation of the esophageal branches of the thoracic aorta.
Resection of the esophagus Separation of the posterior wall of the esophagus from the aorta Crossing and ligation of the esophageal branches of the thoracic aorta.

 Resection of the esophagus Crossing the distal end of the thoracic esophagus Seromuscular interrupted sutures above the mechanical suture line in the cardia area
Resection of the esophagus Crossing the distal end of the thoracic esophagus Seromuscular interrupted sutures above the mechanical suture line in the cardia area


 Posterior mediastinum 1 – a. carotis communis; 2 – esophagus; 3 – n. recurrent; 4 – n. vagus; 5 – a. subclavia; 6 – aortic arch; 7 – left main bronchus; 8 – thoracic aorta; 9 – abdominal esophagus; 10 – a. coeliaca; 11 – diaphragm; 12 – lymph nodes; 13 – 1st rib; 14 – trachea; 15 – larynx; 16 – v. azygos; 17 – thoracic lymphatic duct
Posterior mediastinum 1 – a. carotis communis; 2 – esophagus; 3 – n. recurrent; 4 – n. vagus; 5 – a. subclavia; 6 – aortic arch; 7 – left main bronchus; 8 – thoracic aorta; 9 – abdominal esophagus; 10 – a. coeliaca; 11 – diaphragm; 12 – lymph nodes; 13 – 1st rib; 14 – trachea; 15 – larynx; 16 – v. azygos; 17 – thoracic lymphatic duct




 Drainage of the mediastinum Transcervical mediastinotomy according to V.I. Razumovsky (for injuries of the cervical and upper thoracic esophagus) Transdiaphragmatic mediastinotomy according to Rozanov Savinykh (for injuries of the lower thoracic and abdominal esophagus) Transsternal drainage Extrapleural parasternal drainage with resection of 2 3 costal cartilages according to Madelung u. Transesophageal drainage (while preserving the mediastinal pleura) Transpleural mediastinotomy according to V. D. Dobromyslov (for injuries of the thoracic esophagus with damage to the mediastinal pleura) Posterior extrapleural mediastinotomy according to I. I. Nasilov with resection of several ribs
Drainage of the mediastinum Transcervical mediastinotomy according to V.I. Razumovsky (for injuries of the cervical and upper thoracic esophagus) Transdiaphragmatic mediastinotomy according to Rozanov Savinykh (for injuries of the lower thoracic and abdominal esophagus) Transsternal drainage Extrapleural parasternal drainage with resection of 2 3 costal cartilages according to Madelung u. Transesophageal drainage (while preserving the mediastinal pleura) Transpleural mediastinotomy according to V. D. Dobromyslov (for injuries of the thoracic esophagus with damage to the mediastinal pleura) Posterior extrapleural mediastinotomy according to I. I. Nasilov with resection of several ribs

 Approaches for anterior mediastinitis 1 – cervical mediastinotomy, 2 – suprasternal incision according to Razumovsky, 3 – incision according to Madelung, 4 – transdiaphragmatic mediastinotomy
Approaches for anterior mediastinitis 1 – cervical mediastinotomy, 2 – suprasternal incision according to Razumovsky, 3 – incision according to Madelung, 4 – transdiaphragmatic mediastinotomy


 Topography of the heart The sternocostal surface faces the sternum, costal cartilages, and partly to the mesial pleura. The diaphragmatic surface in the upper sections faces the esophagus and thoracic aorta, and in the lower sections it is adjacent to the diaphragm.
Topography of the heart The sternocostal surface faces the sternum, costal cartilages, and partly to the mesial pleura. The diaphragmatic surface in the upper sections faces the esophagus and thoracic aorta, and in the lower sections it is adjacent to the diaphragm.
 Topography of the heart The sternocostal surface consists of the anterior surfaces of the right atrium, right auricle, superior vena cava, pulmonary trunk, right and left ventricles, as well as the apex of the heart and the apex of the left auricle. The diaphragmatic surface in the upper sections consists of the posterior surfaces of mainly the left and partly the right atria, in the lower sections - the lower surfaces of the right and left ventricles and partly the atria.
Topography of the heart The sternocostal surface consists of the anterior surfaces of the right atrium, right auricle, superior vena cava, pulmonary trunk, right and left ventricles, as well as the apex of the heart and the apex of the left auricle. The diaphragmatic surface in the upper sections consists of the posterior surfaces of mainly the left and partly the right atria, in the lower sections - the lower surfaces of the right and left ventricles and partly the atria.

 Projection of the orifices of the heart onto the anterior wall of the chest. Left atrioventricular orifice to the left of the sternum in the third intercostal space; sounds of the mitral (2 x leaflet valve are heard at the apex of the heart. The right atrioventricular opening behind the right half of the sternum, on a line drawn from the point of connection with the sternum of the cartilage of the left III rib to the point of connection with the sternum of the cartilage of the right VI rib; sounds of 3 x leaflet valve are heard on the right at the level of the cartilages of the V–VI ribs and the adjacent area of the sternum.
Projection of the orifices of the heart onto the anterior wall of the chest. Left atrioventricular orifice to the left of the sternum in the third intercostal space; sounds of the mitral (2 x leaflet valve are heard at the apex of the heart. The right atrioventricular opening behind the right half of the sternum, on a line drawn from the point of connection with the sternum of the cartilage of the left III rib to the point of connection with the sternum of the cartilage of the right VI rib; sounds of 3 x leaflet valve are heard on the right at the level of the cartilages of the V–VI ribs and the adjacent area of the sternum.
 Projection of the openings of the heart onto the anterior wall of the chest. The opening of the aorta is located behind the sternum, closer to its left edge, at the level of the third intercostal space; aortic valve sounds are heard on the right at the edge of the sternum in the second intercostal space. The opening of the pulmonary trunk is located at the level of attachment of the cartilage of the left third rib to the sternum; The tops of the pulmonary valve are heard on the left at the edge of the sternum in the second intercostal space.
Projection of the openings of the heart onto the anterior wall of the chest. The opening of the aorta is located behind the sternum, closer to its left edge, at the level of the third intercostal space; aortic valve sounds are heard on the right at the edge of the sternum in the second intercostal space. The opening of the pulmonary trunk is located at the level of attachment of the cartilage of the left third rib to the sternum; The tops of the pulmonary valve are heard on the left at the edge of the sternum in the second intercostal space.
 Surgical anatomy of the coronary arteries (according to A. A. Shalimov) Right coronary artery: I segment from the mouth to the origin of the artery of the acute edge of the heart (length from 2 to 3.5 cm); II segment from the branch of the acute edge of the heart to the origin of the posterior interventricular branch of the right coronary artery (2, 2, 3, 8 cm); III segment is the posterior interventricular branch of the right coronary artery. Left coronary artery: I segment – from the mouth to the place of division into the main branches II segment – the first 2 cm of the anterior interventricular branch of the left coronary artery III segment – the next 2 cm of the anterior interventricular branch of the left coronary artery IV segment – the distal part of the anterior interventricular branch V segment the circumflex branch of the left coronary artery to the origin of the branch of the obtuse margin of the heart VI segment – distal portion of the circumflex branch of the left coronary artery (artery of the obtuse margin of the heart) VII segment – diagonal branch of the left coronary artery
Surgical anatomy of the coronary arteries (according to A. A. Shalimov) Right coronary artery: I segment from the mouth to the origin of the artery of the acute edge of the heart (length from 2 to 3.5 cm); II segment from the branch of the acute edge of the heart to the origin of the posterior interventricular branch of the right coronary artery (2, 2, 3, 8 cm); III segment is the posterior interventricular branch of the right coronary artery. Left coronary artery: I segment – from the mouth to the place of division into the main branches II segment – the first 2 cm of the anterior interventricular branch of the left coronary artery III segment – the next 2 cm of the anterior interventricular branch of the left coronary artery IV segment – the distal part of the anterior interventricular branch V segment the circumflex branch of the left coronary artery to the origin of the branch of the obtuse margin of the heart VI segment – distal portion of the circumflex branch of the left coronary artery (artery of the obtuse margin of the heart) VII segment – diagonal branch of the left coronary artery

 Types of blood supply to the heart: right coronary type, most parts of the heart are supplied with blood from the branches of the right coronary artery; left coronary type, most of the heart receives blood from the branches of the left coronary artery; medium (uniform) type: both coronary arteries are evenly distributed in the walls of the heart. Transitional types of blood supply to the heart: middle-right, middle-left
Types of blood supply to the heart: right coronary type, most parts of the heart are supplied with blood from the branches of the right coronary artery; left coronary type, most of the heart receives blood from the branches of the left coronary artery; medium (uniform) type: both coronary arteries are evenly distributed in the walls of the heart. Transitional types of blood supply to the heart: middle-right, middle-left
 Arteries of the heart Extraorgan: - right coronary artery (two branches: right marginal and posterior interventricular) - arises from the right sinus of the aortic bulb, supplies blood to the right atrium, part of the anterior and entire posterior walls of the right ventricle, the IVS and part of the IVS; left coronary artery - from the left sinus of the aortic bulb (two branches: anterior interventricular and circumflex - supply blood to the left atrium, part, most of the posterior wall of the LV, part of the anterior wall of the RV, part of the IVS. Intraorgan: arteries of the atrium, cardiac ears, septa, ventricles and papillary muscles.
Arteries of the heart Extraorgan: - right coronary artery (two branches: right marginal and posterior interventricular) - arises from the right sinus of the aortic bulb, supplies blood to the right atrium, part of the anterior and entire posterior walls of the right ventricle, the IVS and part of the IVS; left coronary artery - from the left sinus of the aortic bulb (two branches: anterior interventricular and circumflex - supply blood to the left atrium, part, most of the posterior wall of the LV, part of the anterior wall of the RV, part of the IVS. Intraorgan: arteries of the atrium, cardiac ears, septa, ventricles and papillary muscles.


 Innervation of the heart Nerves: branches of the vagus, sympathetic trunks, phrenic and hypoglossal nerves. Conducting system: Sinus node (lies in the wall of the right atrium). When its integrity is violated, supraventricular arrhythmias of various types occur; Atrioventricular node (Ashofa-Tovar) - in the wall of the RA and through the IVS to the RV and LV.
Innervation of the heart Nerves: branches of the vagus, sympathetic trunks, phrenic and hypoglossal nerves. Conducting system: Sinus node (lies in the wall of the right atrium). When its integrity is violated, supraventricular arrhythmias of various types occur; Atrioventricular node (Ashofa-Tovar) - in the wall of the RA and through the IVS to the RV and LV.

 Congenital heart defects 1. Heart defects with normal blood flow through the lungs coarctation of the aorta according to the adult type 2. Heart defects with increased blood flow through the lungs open ductus arteriosus atrial septal defect ventricular septal defect coarctation of the aorta according to the pediatric type (combined with patent ductus arteriosus - preductal and postductal coarctation) 3. Heart defects with reduced blood flow through the lungs triad, tetrad, pentad of Fallot
Congenital heart defects 1. Heart defects with normal blood flow through the lungs coarctation of the aorta according to the adult type 2. Heart defects with increased blood flow through the lungs open ductus arteriosus atrial septal defect ventricular septal defect coarctation of the aorta according to the pediatric type (combined with patent ductus arteriosus - preductal and postductal coarctation) 3. Heart defects with reduced blood flow through the lungs triad, tetrad, pentad of Fallot


 Aortogram of a patient with coarctation of the aorta According to Abbott statistics, coarctation of the aorta accounts for 14.2% of all congenital heart defects, other authors give a figure of 6.7%. Congenital narrowing of the aorta is located at the junction of the aortic arch and the descending aorta distal to the left subclavian artery.
Aortogram of a patient with coarctation of the aorta According to Abbott statistics, coarctation of the aorta accounts for 14.2% of all congenital heart defects, other authors give a figure of 6.7%. Congenital narrowing of the aorta is located at the junction of the aortic arch and the descending aorta distal to the left subclavian artery.


 Pulmonary valve Located in the fibrous ring in front of the arterial valve. It has 3 pulmonary sinuses and 3 semilunar valves. The diameter of the pulmonary trunk is 2.5 - 3 cm.
Pulmonary valve Located in the fibrous ring in front of the arterial valve. It has 3 pulmonary sinuses and 3 semilunar valves. The diameter of the pulmonary trunk is 2.5 - 3 cm.
 Aortic valve Located in the fibrous ring connected to the membranous part of the IVS. Has 3 semilunar valves, attached to the lower edges of the 3 aortic sinuses; The right coronary artery begins from the right sinus, and the left coronary artery begins from the left sinus; The venom sinus is located extracardially, in contact with the cavity of the transverse sinus of the pericardium
Aortic valve Located in the fibrous ring connected to the membranous part of the IVS. Has 3 semilunar valves, attached to the lower edges of the 3 aortic sinuses; The right coronary artery begins from the right sinus, and the left coronary artery begins from the left sinus; The venom sinus is located extracardially, in contact with the cavity of the transverse sinus of the pericardium
 Indirect cardiac revascularization 1. The organopexy method involved suturing vessels of nearby organs (lung, diaphragm, omentum) to the heart. 2. Talc was poured into the pericardial cavity; pericarditis developed with the formation of adhesions; in the adhesions, the vessels approached the walls of the heart. 3. 1939 Fieski 2-sided dressing and cutting a. thoracica interna. This leads to an increase in blood flow in a. pericarodiaca phrenica (by 20%). Also an ineffective method. 4. 1945 Weinberg direct implantation a. Thoracica interna into the thickness of the myocardium: blood passes through the tunnel between the muscle fibers and subsequently collaterals develop. Used for diffuse lesions of the coronary arteries.
Indirect cardiac revascularization 1. The organopexy method involved suturing vessels of nearby organs (lung, diaphragm, omentum) to the heart. 2. Talc was poured into the pericardial cavity; pericarditis developed with the formation of adhesions; in the adhesions, the vessels approached the walls of the heart. 3. 1939 Fieski 2-sided dressing and cutting a. thoracica interna. This leads to an increase in blood flow in a. pericarodiaca phrenica (by 20%). Also an ineffective method. 4. 1945 Weinberg direct implantation a. Thoracica interna into the thickness of the myocardium: blood passes through the tunnel between the muscle fibers and subsequently collaterals develop. Used for diffuse lesions of the coronary arteries.
 Direct cardiac revascularization 1. 1960 mammary coronary anastomosis – highlighted a. thoracica interna and is sutured into the coronary artery distal to the lesion. Demikhov V.P. experiment. In 1967, the same operation was performed on a human by Kolesov. 2. 1967 – Favaloro aortocoronary bypass surgery.
Direct cardiac revascularization 1. 1960 mammary coronary anastomosis – highlighted a. thoracica interna and is sutured into the coronary artery distal to the lesion. Demikhov V.P. experiment. In 1967, the same operation was performed on a human by Kolesov. 2. 1967 – Favaloro aortocoronary bypass surgery.


 Endovascular interventions 1978 Grünzig. 1. Balloon dilation of the coronary artery ostium under local anesthesia using a catheter tip during coronary angiography. The effect persists for 3 years. 2. Chazov administers thrombolytics through a catheter. 3. Laser photocoagulation laser light guide, at the end there is a sapphire tip (heated to 400 (C), it is touched to the plaque.
Endovascular interventions 1978 Grünzig. 1. Balloon dilation of the coronary artery ostium under local anesthesia using a catheter tip during coronary angiography. The effect persists for 3 years. 2. Chazov administers thrombolytics through a catheter. 3. Laser photocoagulation laser light guide, at the end there is a sapphire tip (heated to 400 (C), it is touched to the plaque.

 Mitral stenosis (narrowing of the left atrioventricular orifice) stenosis in the form of a “jacket loop” - thickening and mild fusion of the leaflets (commissurotomy is possible) stenosis in the form of a “fish mouth” - pronounced fusion with changes in the subvalvular apparatus (valve replacement is required)
Mitral stenosis (narrowing of the left atrioventricular orifice) stenosis in the form of a “jacket loop” - thickening and mild fusion of the leaflets (commissurotomy is possible) stenosis in the form of a “fish mouth” - pronounced fusion with changes in the subvalvular apparatus (valve replacement is required)
 Ball mechanical artificial heart valves (MIX) Starr-Edwards valve - the first MIX interferes with blood flow Starr-Edwards valve
Ball mechanical artificial heart valves (MIX) Starr-Edwards valve - the first MIX interferes with blood flow Starr-Edwards valve

 Disc mechanical artificial heart valves Bicuspid valve Sant Jude Medical - Regent Valve Med. Eng.
Disc mechanical artificial heart valves Bicuspid valve Sant Jude Medical - Regent Valve Med. Eng.
 Biological artificial heart valves (BIHS) Supported valve: Porcine Carpentier Edwards valve Carpentier Edwards pericardial valve Supported valve: Toronto valve Porcine Freestyle valve
Biological artificial heart valves (BIHS) Supported valve: Porcine Carpentier Edwards valve Carpentier Edwards pericardial valve Supported valve: Toronto valve Porcine Freestyle valve

 Suturing a heart wound in the area of the coronary artery with a U-shaped suture to avoid ligation of the coronary arteries
Suturing a heart wound in the area of the coronary artery with a U-shaped suture to avoid ligation of the coronary arteries


 Segmental structure of the right lung (mediastinal surface) Upper lobe SI segmentum apicale; SII segmentum posterius; SIII segmentum anterius. Middle lobe SIV segmentum laterale; SV segmentum mediale. Lower lobe SVI segmentum apicale; SVII segmentum basale mediale (cardiacum) SVIII segmentum basale anterius; SIX segmentum basale laterale; SX segmentum basale posterius.
Segmental structure of the right lung (mediastinal surface) Upper lobe SI segmentum apicale; SII segmentum posterius; SIII segmentum anterius. Middle lobe SIV segmentum laterale; SV segmentum mediale. Lower lobe SVI segmentum apicale; SVII segmentum basale mediale (cardiacum) SVIII segmentum basale anterius; SIX segmentum basale laterale; SX segmentum basale posterius.
 Segmental structure of the left lung (mediastinal surface) Upper lobe SI+II segmentum apicoposterius; SIII segmentum anterius; SIV segmentum lingulare superius; SV segmentum lingulare inferius. Lower lobe SVI segmentum apicale; SVII segmentum basale mediale (cardiacum) SVIII segmentum basale anterius; SIX segmentum basale laterale; SX segmentum basale posterius.
Segmental structure of the left lung (mediastinal surface) Upper lobe SI+II segmentum apicoposterius; SIII segmentum anterius; SIV segmentum lingulare superius; SV segmentum lingulare inferius. Lower lobe SVI segmentum apicale; SVII segmentum basale mediale (cardiacum) SVIII segmentum basale anterius; SIX segmentum basale laterale; SX segmentum basale posterius.



 The roots of the lung in the horizontal plane Anteriorly - the pulmonary veins Behind them - the branches of the pulmonary artery Most posteriorly - the main bronchus (surrounded by the branches of the vagus nerve and the sympathetic trunk)
The roots of the lung in the horizontal plane Anteriorly - the pulmonary veins Behind them - the branches of the pulmonary artery Most posteriorly - the main bronchus (surrounded by the branches of the vagus nerve and the sympathetic trunk)
 Resection interventions on the lungs Wedge-shaped resection of the lung (with the application of a continuous continuous suture); Removal of a segment of the lung (segmentectomy; Removal of a lobe of the lung (lobectomy); Removal of the lung (pneumonectomy); Suturing of the wound of the main bronchi (wedge-shaped excision, end-to-end anastomosis).
Resection interventions on the lungs Wedge-shaped resection of the lung (with the application of a continuous continuous suture); Removal of a segment of the lung (segmentectomy; Removal of a lobe of the lung (lobectomy); Removal of the lung (pneumonectomy); Suturing of the wound of the main bronchi (wedge-shaped excision, end-to-end anastomosis).
 Pulmonectomy Displacement of tissue and lymph nodes, intersection of the pericardial arterial ligament Treatment of the main vessels of the root of the right lung
Pulmonectomy Displacement of tissue and lymph nodes, intersection of the pericardial arterial ligament Treatment of the main vessels of the root of the right lung
 Pulmonectomy Intersection of the main bronchus leaving one cartilaginous semi-ring Suturing the stump of the main bronchus with interrupted sutures on atraumatic needles
Pulmonectomy Intersection of the main bronchus leaving one cartilaginous semi-ring Suturing the stump of the main bronchus with interrupted sutures on atraumatic needles
 Errors and dangers of operations on the lungs In 34% of cases, the arteries of the 4th and 5th segments arise SEPARATELY from the interlobar artery. When removing the middle lobe, the middle lobe bronchus is first crossed, and then the artery; With atypical outflow of the veins of segments 3 and 4, complications may arise when isolating the upper and lower pulmonary veins during resection of the middle and upper lobes of the right lung; In case of atypical origin of the arteries of the 3rd segment from the upper trunk, resection of the lingular segments is dangerous; With a mixed type of venous outflow (the vein of the first segment flows into the vein of the third), damage to the veins of the 3rd segment is dangerous. The drainage of the veins of the lingular segments into the inferior pulmonary vein can lead to erroneous ligation of the veins of the 3rd segment instead of the veins of the 4th and 5th segments
Errors and dangers of operations on the lungs In 34% of cases, the arteries of the 4th and 5th segments arise SEPARATELY from the interlobar artery. When removing the middle lobe, the middle lobe bronchus is first crossed, and then the artery; With atypical outflow of the veins of segments 3 and 4, complications may arise when isolating the upper and lower pulmonary veins during resection of the middle and upper lobes of the right lung; In case of atypical origin of the arteries of the 3rd segment from the upper trunk, resection of the lingular segments is dangerous; With a mixed type of venous outflow (the vein of the first segment flows into the vein of the third), damage to the veins of the 3rd segment is dangerous. The drainage of the veins of the lingular segments into the inferior pulmonary vein can lead to erroneous ligation of the veins of the 3rd segment instead of the veins of the 4th and 5th segments
 Suturing lung wounds Access: anterolateral or lateral thoracotomy along the IV–V intercostal spaces. Operations: for stab wounds - interrupted sutures. For linear wounds of more than 1 cm - a crucible suture. Bronchial wounds are stitched with atraumatic needles. For a gunshot wound, a segment, forehead, or pneumonectomy are used.
Suturing lung wounds Access: anterolateral or lateral thoracotomy along the IV–V intercostal spaces. Operations: for stab wounds - interrupted sutures. For linear wounds of more than 1 cm - a crucible suture. Bronchial wounds are stitched with atraumatic needles. For a gunshot wound, a segment, forehead, or pneumonectomy are used.

 Layers of the chest wall superficial layer - skin, subcutaneous tissue and mammary gland muscular-fascial layer - in front - pectoralis major and minor muscles, on the side - serratus anterior muscles, behind - latissimus dorsi deep layer - intercostal muscles and osteochondral base
Layers of the chest wall superficial layer - skin, subcutaneous tissue and mammary gland muscular-fascial layer - in front - pectoralis major and minor muscles, on the side - serratus anterior muscles, behind - latissimus dorsi deep layer - intercostal muscles and osteochondral base

 Superficial layer of the chest wall The skin is thin, contains hair follicles, sweat and sebaceous glands (when the excretory ducts are blocked, atheromas develop); Subcutaneous fatty tissue contains superficial vessels: branches of the posterior intercostal arteries (from the aorta), anterior intercostal arteries (from the internal thoracic artery) and lateral thoracic arteries (from the axillary artery); Superficial fascia extends from the collarbone and forms the capsule for the mammary gland (ligament that supports the mammary gland)
Superficial layer of the chest wall The skin is thin, contains hair follicles, sweat and sebaceous glands (when the excretory ducts are blocked, atheromas develop); Subcutaneous fatty tissue contains superficial vessels: branches of the posterior intercostal arteries (from the aorta), anterior intercostal arteries (from the internal thoracic artery) and lateral thoracic arteries (from the axillary artery); Superficial fascia extends from the collarbone and forms the capsule for the mammary gland (ligament that supports the mammary gland)
 Deep layer of the chest wall Osteocartilaginous base: sternum (manubrium, body and xiphoid process), spine (I - XII thoracic vertebrae), ribs. Intercostal spaces: external intercostal muscles (do not reach the sternum), internal intercostal muscles (run from the sternum to the costal angles behind) between the muscles - intercostal vessels, nerve (in the groove the ribs go to the mid-axillary line) and lymphatic vessels. Puncture of the sternum: in the midline at the level of the first ribs
Deep layer of the chest wall Osteocartilaginous base: sternum (manubrium, body and xiphoid process), spine (I - XII thoracic vertebrae), ribs. Intercostal spaces: external intercostal muscles (do not reach the sternum), internal intercostal muscles (run from the sternum to the costal angles behind) between the muscles - intercostal vessels, nerve (in the groove the ribs go to the mid-axillary line) and lymphatic vessels. Puncture of the sternum: in the midline at the level of the first ribs

 Classification of mastitis Acute Chronic galactophoritis (inflammation of the milk ducts) areolitis (inflammation of the glands near the nipple circle) diffuse purulent: characterized by the formation of small abscesses and pronounced induration of the surrounding tissue; plasma cell (non-purulent): mammography, cytological examination of punctate, histological examination of removed tissues are mandatory. If conservative treatment is ineffective within 2 weeks, sectoral resection is performed.
Classification of mastitis Acute Chronic galactophoritis (inflammation of the milk ducts) areolitis (inflammation of the glands near the nipple circle) diffuse purulent: characterized by the formation of small abscesses and pronounced induration of the surrounding tissue; plasma cell (non-purulent): mammography, cytological examination of punctate, histological examination of removed tissues are mandatory. If conservative treatment is ineffective within 2 weeks, sectoral resection is performed.
 Classification of mastitis depending on location 1 subareolar 2 intramammary 3 – premammary (subcutaneous) 4 retromammary
Classification of mastitis depending on location 1 subareolar 2 intramammary 3 – premammary (subcutaneous) 4 retromammary
 Classification of mastitis depending on the stage of the inflammatory process serous (initial) infiltrative infiltrative purulent (apostematous like a “honeycomb”) abscessing phlegmonous gangrenous
Classification of mastitis depending on the stage of the inflammatory process serous (initial) infiltrative infiltrative purulent (apostematous like a “honeycomb”) abscessing phlegmonous gangrenous

 Pericardial puncture - Larrey's point between the xiphoid process and the left costal arch (cartilaginous surface of the VII rib); Marfan's point under the apex of the xiphoid process; Pirogov's Karavaev point in the fourth intercostal space on the left, 2 cm outward from the sternum. Delorme Mignon's point in the sixth intercostal space on the left at the sternum
Pericardial puncture - Larrey's point between the xiphoid process and the left costal arch (cartilaginous surface of the VII rib); Marfan's point under the apex of the xiphoid process; Pirogov's Karavaev point in the fourth intercostal space on the left, 2 cm outward from the sternum. Delorme Mignon's point in the sixth intercostal space on the left at the sternum  Breast cancer (lymphogenous metastasis) axillary scapular subclavian lymph nodes; parasternal, supraclavicular, cervical and l/a mediastinum (central cancer); cross metastasis (axillary nodes of the opposite side); distant metastasis: vertebral bodies, pelvic bones, lung, liver, brain, etc.
Breast cancer (lymphogenous metastasis) axillary scapular subclavian lymph nodes; parasternal, supraclavicular, cervical and l/a mediastinum (central cancer); cross metastasis (axillary nodes of the opposite side); distant metastasis: vertebral bodies, pelvic bones, lung, liver, brain, etc.
 Simple mastectomy (Maden operation) - the entire mammary gland is removed; regional axillary lymph nodes are not removed; the pectoralis major and minor muscles are not removed.
Simple mastectomy (Maden operation) - the entire mammary gland is removed; regional axillary lymph nodes are not removed; the pectoralis major and minor muscles are not removed.
 Radical mastectomy (Halstead operation) - the entire mammary gland is removed, regional axillary lymph nodes are removed, the pectoralis major and minor muscles are removed, the long thoracic nerve is left The operation leads to severe deformation of the chest
Radical mastectomy (Halstead operation) - the entire mammary gland is removed, regional axillary lymph nodes are removed, the pectoralis major and minor muscles are removed, the long thoracic nerve is left The operation leads to severe deformation of the chest





Rib cage- the bone base of the chest walls. Consists of XII thoracic vertebrae, XII pairs of ribs and sternum.
Chest walls:
The posterior wall is formed by the thoracic part of the spinal column, as well as the posterior sections of the ribs from the head to their corners.
The anterior wall is formed by the sternum and the cartilaginous ends of the ribs.
The lateral walls are formed by the bony part of the ribs.
The upper aperture of the chest is limited by the posterior surface of the manubrium of the sternum, the inner edges of the first ribs and the anterior surface of the first thoracic vertebra.
The lower aperture of the chest is limited by the posterior surface of the xiphoid process of the sternum, the lower edge of the costal arch, and the anterior surface of the X thoracic vertebra. The lower aperture is closed by a diaphragm.
Skeleton of the chest, a - front view. 1 - upper thoracic aperture; 2 - jugular
tenderloin; 3 - manubrium of the sternum; 4 - body of the sternum; 5 - xiphoid process of the sternum; 6 - oscillating ribs (XI-XII); 7 - substernal angle; 8 - lower thoracic aperture; 9 - false ribs (VIII-X); 10 - costal cartilages; 1 1 - true ribs (I-VII); 12 - collarbone.
Topography of intercostal spaces.
Topography of the intercostal neurovascular bundle on the posterior and anterior surfaces of the chest  :
:
I – between the middle axillary and paravertebral lines;
II - between the middle axillary and midclavicular lines.
1 – fascia m. latissimusdorsi; 2 – m. latissimusdorsi; 3 – fascia thoracica; 4 – v. intercostalis;
5 – a. intercostalis; 6 – n. intercostalis; 7 – m. Intercostalisexternus; 8 – m. intercostalisinternus;
9 – fasciaendothoracica; 10 – prepleural tissue; 11 – pleura parietalis;
12 – fasciapectoralis; 13 - m. pectoralis major.
In the spaces between the ribs there are external and internal intercostal muscles, fiber and neurovascular bundles.
External intercostal muscles (mm. intercostalisexterni) go from the lower edge of the ribs obliquely from top to bottom and anteriorly to the upper edge of the underlying rib. At the level of the costal cartilages, muscles are absent and replaced by the outer intercostal membrane.
Internal intercostal muscles (mm. intercostales interni) go obliquely from bottom to top and back. Posterior to the costal angles, muscle bundles are absent and replaced by an internal intercostal membrane.
The space between adjacent ribs, limited externally and internally by the corresponding intercostal muscles, is called the intercostal space. It contains a vein, below it is an artery, and even lower is a nerve.
Posterior intercostal arteries(IX-X pairs) extend from the aorta, located in the intervals from the III to the XI ribs, the twelfth artery, lying under the XII rib, is called the subcostal artery (a. subcostalis). Branches:
· Dorsal branch (r. dorsalis) goes to the muscles and skin of the back
· Lateral and medial cutaneous branches (r. cutaneus lateraliset medialis) go to the skin of the chest and abdomen
· Lateral and medial branches of the mammary gland (rr. mammariilateraliset medialis)
15129 0
The chest wall is divided into three layers: superficial, middle and deep. The layers of the chest wall are best identified in horizontal cuts of the body (Fig. 2, 3), introduced into the practice of topographic anatomy by N.I. Pirogov. The superficial layer includes the skin, mammary gland, subcutaneous fatty tissue, as well as the vessels and nerves supplying the formations of this layer. The middle layer contains the muscles covering the chest wall (Fig. 4, 5). The deep layer is formed by the ribs, intercostal muscles, ligaments, vessels and nerves.
Rice. 2. Topography of the organs of the thoracic cavity, a - horizontal cut at the level of Th3-5: 1 - axillary cavity with vessels and nerves; 2 - right lung; 3 - pectoralis minor muscle; 4 - pectoralis major muscle; 5 - cartilaginous part of the first rib; 6 - collarbone. 7 - manubrium of the sternum; 8 - intercostal muscles; 9 - left lung; 10 - blade; 11 - infraspinatus muscle; 12 - erector spinae muscle; 13 - semispinalis muscle of the neck. 14 - III thoracic vertebra; 15 - trapezius muscle; 16-subscapularis muscle; 17 deltoid muscle; 18 - humerus; 19 - tendon of the long head of the biceps muscle. b - topography of the thoracic cavity organs, horizontal cut at the level of Th5-7: 1 - deltoid muscle; 2 - coracobrachialis muscle; 3 - axillary cavity with vessels and nerve; 4 - internal mammary artery and vein; 5 - sternum; 6 - cartilaginous part of the 2nd rib; 7 - pectoralis minor muscle; 8 - pectoralis major muscle; 9 - left lung; 10 - humerus; 11 - teres major muscle; 12 - shoulder blade muscle; 13 - infraspinatus muscle; 14 - rectifier muscle; 15 - intervertebral disc; 16 - trapezius muscle; 17 - rhomboid major muscle; 18 - right lung; 19 - triceps brachii muscle.

Rice. 3. Topography of the thoracic cavity organs, a - horizontal cut at the Th7 level. 1 - pectoralis major muscle; 2 - sternum; 3 - internal thoracic artery and vein; 4 - heart; 5 - left lung; 6 - serratus anterior muscle; 7 - latissimus dorsi; 8 - lower angle of the scapula; 9 - erector spinae muscle; 10 - trapezius muscle; 11 - VII thoracic vertebra; 12 - “auscultation triangle”; 13 - intercostal muscles. b - horizontal cut at level Th10. 1 - rectus abdominis muscle; 2 - costal part of the diaphragm; 3 - xiphoid process; 4 - cartilaginous part of the ribs; 5 - stomach; 6 - aorta; 7 - spleen; 8 - lower lobe of the left lung; 9 - erector spinae muscle; 10 - X thoracic vertebra; 11 - trapezius muscle; 12 - right lung; 13 - latissimus dorsi muscle; 14 - serratus anterior muscle; 15 - liver.

Rice. 4. Muscles of the anterior chest wall, their blood supply and innervation. 1 - cephalic vein; 2 - arteries of the chest and brachial process; 3 - dorsal artery of the scapula; 4 - transverse artery of the neck. 5 - subclavian artery and vein; 6 - thoracic artery; 7 - the uppermost artery of the chest; 8 - anterior thoracic nerve; 9 - lateral artery of the chest; 10 - long thoracic nerve; 11 - posterior thoracic artery; 12 - artery surrounding the scapula; 13 - main ulnar saphenous vein; 14 - cutaneous dorsal nerve of the forearm; 15 brachial artery; 16th median nerve; 17th ulnar nerve; 18 musculocutaneous nerve.

Rice. 5. Muscles of the posterior surface of the chest wall.
1 - trapezius muscle; 2 - sternocleidomastoid muscle; 3 - semispinalis capitis muscle; 4 - splenius capitis muscle; 5 - muscle that lifts the scapula; 6 - supraspinatus muscle; 7 - rhomboid minor muscle; 8 - rhomboid major muscle; 9 - teres major muscle; 10 - latissimus dorsi; 11 - rectifier muscle; 12-inferior posterior serratus muscle; 13 - external oblique abdominal muscle; 14- teres minor muscle; 15 - infraspinatus muscle; 16 - deltoid muscle.
The skin on the anterior and lateral surfaces of the chest wall is thinner than in the back and contains sebaceous and sweat glands. Under the skin there is a layer of fiber, expressed individually. In the area of the sternum and spinous processes, the fiber is poorly developed, penetrated by connective tissue bridges, as a result of which the skin is inactive. In the area of the nipple and areola of the mammary glands, there is no fiber and the skin of these areas is motionless. Superficial vessels and nerves pass through the subcutaneous tissue.
The arteries are branches of the intercostal, axillary, lateral thoracic arteries and the internal mammary artery (Fig. 6). The veins of the chest wall (Fig. 7) form a thin subcutaneous network, especially pronounced in the area of the mammary glands. The saphenous veins are connected by perforating branches to the axillary, subclavian, intercostal and internal mammary veins, as well as the veins of the anterior abdominal wall. The anterior and posterior branches of the thoracic nerves branch in the subcutaneous tissue. The superficial branches of the medial supraclavicular nerves from the cervical plexus pass here.

Rice. 6. Arteries of the chest wall.
1 - thoracic aorta; 2 - intercostal arteries; 3 - internal mammary artery; 4 - upper costal branch of the intercostal artery; 5 - lower costal branch of the intercostal artery; 6 - posterior branch of the intercostal artery.

Rice. 7. Veins of the anterior chest wall.
1 - radial saphenous vein (cephalic vein); 2 - subalacular vein; 3 - subclavian vein; 4 - external jugular vein; 5 - internal jugular vein; 6 - anterior jugular vein; 7 - sterno-epigastric vein; 8 - internal mammary vein; 9 - lateral thoracic vein; 10 - ulnar saphenous vein (main vein).
A.A. Vishnevsky, S.S. Rudakov, N.O. Milanov
Topographic anatomy and operative surgery of the chest walls, breast
TOPOGRAPHIC ANATOMY OF THE BREAST
Borders
The upper border of the chest is drawn from the jugular notch of the sternum along the clavicle to the articulation between the clavicle and the acromial process of the scapula; from here a straight line is drawn to the spinous process of the VII cervical vertebra (Fig. 1).
Rice. 1. Chest area
1 – thoracic region, 2 – presternal region, 3 – subthoracic region, 4 – subscapular region, 5 – vertebral region, 6 – scapular region. (From: Shevkunenko V.N. Short course of operative surgery with topographic anatomy. - M., 1951.)
The lower border is drawn from the xiphoid process along the edge of the costal arch to the X rib, from here through the ends of the XI-XII ribs to the spinous process of the XII thoracic vertebra.
Thorax and chest cavity
The thoracic skeleton consists of the thoracic spine, 12 pairs of ribs and the sternum. The lower opening of the chest - aperture thoracis inferior - is closed by a diaphragm, through the openings of which the esophagus, vessels and nerves pass. The superior opening - aperture thoracis superior - allows organs going to or from the neck to pass through; through the upper opening, the apex of the lung, covered with a dome of pleura, protrudes into the neck area on the right and left. The space bounded by the chest and diaphragm is called the chest cavity (cavum pectoris); The diaphragm separates the chest cavity from the abdominal cavity.
It should be noted that the dimensions of the thoracic cavity are inferior to the dimensions of the chest, since from the side of the abdomen the organs that perform the right and left hypochondrium (liver, stomach, spleen) protrude.
Within the chest cavity there are three serous sacs: two pleural and pericardial. In addition, in the chest cavity there is a mediastinum containing a complex of organs, incl. and heart with pericardium.
External landmarks
In front, within the chest, identification points are the following bone formations:
1. Clavicles.
2. Ribs and costal arches. The first rib can be felt only near its attachment to the sternum below the collarbone. Down from the middle of the clavicle, the second rib is felt first. Therefore, the second rib is used as a reference point when counting, conventionally taking the clavicle as the first rib. The first rib is attached to the sternum at the level of the junction of the manubrium and the body of the sternum.
On the side of the xiphoid process of the sternum, the costal arch begins, formed by the cartilages of the VII-X ribs. Only the cartilage of the 7th rib is directly related to the xiphoid process: it connects to the notch located at the border of the body of the sternum and the base of the xiphoid process.
3. The sternum can be palpated along its entire length, and the junction of the manubrium with the body often forms a protrusion - the sternal angle (angulus sternalis).
The upper border of the sternum is located at the level of the lower edge of the II thoracic vertebra, angulus sternalis, corresponding to the level of the intervertebral cartilage between the IV and V thoracic vertebrae. The lower end of the body of the sternum corresponds to the X thoracic vertebra, and the apex of the xiphoid process corresponds to the XI thoracic vertebra.
4. The coracoid process of the scapula (processus coracoideus) is palpable in the subclavian fossa.
Above the sternum there is the suprasternal (or jugular) fossa (fossa jugularis), below the sternum there is the substernal or epigastric (otherwise known as the epigastric) fossa (fossa epigastrica; scrobiculus cordis - BNA).
The intercostal spaces are wider in front than in the back; the widest of them is the third. The nipple in men usually corresponds to the fourth intercostal space. In women, the position of the nipple is very variable.
Muscle outlines may be noticeable in people who are thin or have well-developed muscles. In particular, the pectoralis major muscle protrudes from the front; On the lateral surface of the chest, a zigzag line formed by the teeth of the serratus anterior and external oblique abdominal muscles (Gerdi's line) can be noticeable.
The cardiac impulse is determined in the left fifth intercostal space, 1.5-2.0 cm inward from the line passing through the middle of the clavicle.
To determine the projection of the lungs, heart and abdominal organs, conditional lines are drawn on the chest.
On the anterior surface of the chest:
1. anterior median line - linea mediana anterior - is drawn from the jugular notch, along the middle of the sternum, through the navel to the symphysis;
2. sternal (or sternal) line, right and left – linea sternalis dextra and sinistra – is drawn along the corresponding edge of the sternum;
3. peri-sternal (or parasternal) line, right and left – linea parasternalis dextra and sinistra – is drawn in the middle of the distance between the sternum and nipple line;
4. nipple line – linea mamillaris – is drawn through the nipple. However, the position of the nipples is changeable, so they often use a line drawn through the middle of the clavicle - it is called linea medioclavicularis (mid-clavicular line).
On the lateral surface of the chest:
5) front;
6) average;
7) posterior axillary lines - linea axillaris anterior, media and posterior - are drawn down from the anterior edge of the axillary fossa (anterior line), the deepest point of the fossa (midline) and from the posterior edge (posterior line).
On the back surface of the chest are carried out:
8) posterior median line – linea mediana posterior – along the spinous processes of the vertebrae;
9) vertebral line, right and left – linea vertebralis dextra and sinistra – through the transverse processes of the vertebrae;
10) paravertebral (or paravertebral) line, right and left – linea paravertebralis dextra and sinistra – between the vertebral and scapular line;
11) scapular line, right and left – linea scapularis dextra and sinistra – through the lower angle of the scapula (with a pubescent arm).
The scapula covers the posterior surface of the chest from the upper edge of the 2nd rib to the upper edge of the 7th rib. The horizontal line connecting the lower angles of the shoulder blades passes through the spinous process of the VII thoracic vertebra.
New articles
- Training at the school for foster parents remotely and on weekends for adoption and acceptance of a child into a new family
- Mask with activated carbon and milk
- What causes stomach pain during pregnancy?
- Making fun paper applications with your kids
- Children's aggression: advice from a psychologist
- Knitting toys Legs - orange thread
- New Year's stencils for cutting out paper Openwork Santa Claus
- How to professionally blow dry short hair at home
- How to make animals from beads
- Origami paper balls for the New Year Flower paper ball
Popular articles
- Air Beads Materials and Tools
- How to knit baby booties?
- Can a pregnant woman sleep on her back?
- Is it possible to eat chalk during pregnancy?
- Strawberry allergy, treatment
- Why you shouldn’t hit children Which parenting model to choose
- DIY paper lunar rover
- Why do babies need complementary foods?
- I'm alone on New Year's Day. New Year alone. What to do. Psychological tips for defeating loneliness
- Hair styler - where to buy, reviews